Skin fungal infections are a problem millions of people worldwide deal with several times throughout their lifetime despite scientific advancements.
Fungi infecting the skin often show no symptoms up until the infection installs and spreads, while the most common symptom exhibited when suffering from a fungal infection is itching, often accompanied by redness.
There are many risk factors for fungal infections, but the trigger is almost always lack of proper hygiene.
For this reason, we are all at risk of contracting a fungal infection of the skin at some point in our lives. People with weak immunity, namely HIV or AIDS sufferers, chemotherapy patients, the elderly and children are the categories most at risk due to poor immunity. Similarly, antibiotic use increases the chances of fungal infections as a result of destroying good bacteria cultures in our body.

What is a fungal skin infection?
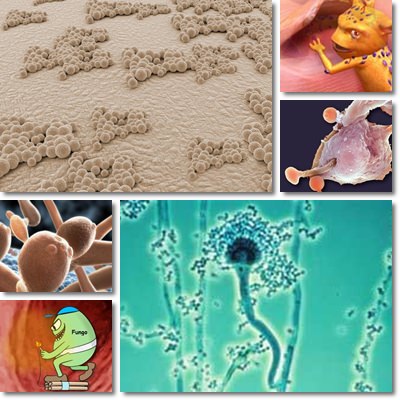
This is a particular type of skin infection produced by microorganisms called fungi such as molds or yeasts. Mushrooms too are a type of fungus, but a multicellular one. In other words, they are made up of billions of cells that allow for them to be seen clearly by the human eye, without the help of a microscope. Fungi grow by decomposing things around them and absorbing food from the outside world, hence their spread when infecting the skin. But not all fungi are parasitic.
There are good fungi as well. Leavening bread, fermenting soy sauce, wine or other beverages, producing antibiotics are all great ways in which fungi prove useful to us. Nevertheless, contracting a fungal infection of the skin is not at all beneficial for us because we end up having a parasitic unicellular microorganism living off us whilst producing unwanted side effects.
When we say skin fungus, skin mycosis or any phrase referring to a fungus-caused infection of the skin, most of us immediately think about toenail fungus infections which cause the nail to become yellow, frail, thick and the area around it red and itchy.
Unfortunately, there is much more to the issue as skin fungal infections can appear almost anywhere on the body and exhibit a variety of symptoms. For example, Tinea versicolor, a skin condition causing whitish, pale, pink or tan spots on the face, chest and arms is also caused by a fungal infection.
Sources of transmission Of Skin Fungal
1) Direct contact with the skin of an infected person as long as the fungus is transmissible. Some are not.
2) Walking barefoot or touching surfaces touched or walked on by people with skin fungal infections.
3) Warm, humid places such as saunas, swimming pools, gyms, locker rooms at school or at the gym or any warm, humid public places.
4) Contaminated pieces of clothing (socks, t-shirts, underwear).
5) Lack of proper hygiene. Perspiration, walking barefoot or exposing skin areas. Infection is highly dependent on the type of fungus.
6) Poor immunity. This is especially true for people with compromised immunity or an underactive immune system.
7) Antibiotic use or overuse. Antibiotics destroy good bacteria, disrupting the body’s microflora balance and allowing for bad bacteria to take control.
8) Not washing up and not changing clothes following intense physical exercises.
9) Synthetic fabrics: acrylic, nylon, spandex, latex, rayon, etc.
10) Scratches from cats that live outdoors and tend to roam a lot.
Others transmission of skin fungal are:
Some types of fungi inhabiting the skin are transmissible from person to person, clothing item to person, surface to person, others infect through spores which are inhaled via air while some develop by themselves as a result of humidity and other encouraging factors.
Perspiration, synthetic clothing, not washing up following intense physical exercise will not necessarily lead to skin fungal infections, but they increase the chances of a perfectly healthy person getting them.
Similarly, touching a person with a skin fungus may be perfectly harmless because it depends on whether or not the fungus is transmissible via touch.
Very important: most skin infections occur in places where skin meets skin, such as between the toes or in between skin folds. This also explains why people suffering from morbid obesity develop infections in between skin folds where there is moisture and warmth to favor fungal growth.
Those at greater risk for developing fungal infections are those with immune system problems:
1) HIV or AIDS sufferers.
2) Chemotherapy patients.
3) Diabetes sufferers.
4) People suffering from obesity.
5) Children and the elderly.
Types of fungus infections
Fungal infections of the skin differ according to the level of the skin the fungus inhabits and are classified as follows:
1) Superficial mycosis
This means the infection occurs at the outermost layers of the skin. It can occur in perfectly healthy individuals, usually on areas such as legs, feet, arms, hands or torso.
2) Cutaneous mycosis
In this case, the fungal infections go deeper into the first layer of the skin and may affect nails and hair as well. Nails funguses, athlete’s foot, tinea or ringworm (causing circular, ring-like rashes), etc.
3) Subcutaneous mycosis
They occur at the level of the dermis, a lower skin levels and even under tissues or muscles. While the first two may be treated fairly easily, fungal infections under the skin are very difficult to treat.
4) Systemic mycoses due to primary pathogens
The types of fungi causing such infections may go from unicellular to multicellular and often become more aggressive as the infection spreads. They usually occur in the lungs and spread from there if left untreated.
5) Systemic mycoses due to opportunistic pathogens
This category includes people with compromised immunity as a result of AIDS, final stages of cancer, chemotherapy, immune suppression medication (corticosteroid medication), antibiotics, etc. The Aspergillus fungus, for example, may infect the lining of the lungs or the brain and cause chronic obstructive pulmonary disease, tuberculosis or meningitis.
5 Prevention Tips For Skin Fungal
Prevention is the best treatment for skin fungal infections as well as other types of fungal infections. Generally, good personal hygiene and avoiding sharing personal objects make the biggest difference.
Here are my 5 tips for preventing fungal infections:
1) Keep clean
Proper personal hygiene is pivotal for avoiding any kind of infection and most diseases. Avoid sharing personal objects such as toothbrushes, combs, towels, socks, underwear, soap, razor blades, summer shoes especially, bed linen, etc. It might also be good to avoid over-crowded swimming pools, public showers used by a great number of people every day and wear shoes at all time instead of walking barefoot in such places.
2) Use fabrics that let the skin breathe
Avoid synthetic fabric such as nylon, acrylic or latex. Instead go for cotton. Unlike synthetic fabrics which keep moisture in, cotton lets the skin breathe properly and prevents moisture that may lead to skin fungal infections. It is recommended to use cotton bed linen, pillow cases, underwear, etc.
3) Avoid spoilt foods
Improper storage and keeping foods well beyond their expiration date will result in them developing molds and becoming improper for eating. While penicillin has been extracted from a mold, eating moldy foods will cause you to get sick.
4) Keep hydrated and take your vitamins
Drinking liquids helps replace what is lost through perspiration and urine and keeps the body working well. Vitamins as well as dietary minerals supports the immune function and do not allow for fungal infections to take place.
If you suspect you have contracted any sort of fungal infection, talk to your doctor so he or she can prescribe you appropriate treatment.
Types of antifungal medication your doctor may prescribe you are:
1) Topical antifungals, applied directly to the affected area.
2) Oral antifungals or medication taken via mouth in the form of capsules, tablets or liquids.
3) Intravenous antifungals. They are only prescribes in severe cases and are administered by a medical professional.
